How to Reduce Pain and Spot Warning Signs of Arthritis in Your Feet
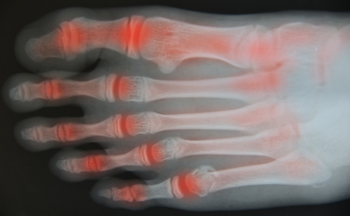
Arthritis is a degenerative condition that causes pain and inflammation in the joints which can worsen over time. Osteoarthritis is a result of damage to cartilage which leads to bone on bone grinding, whereas rheumatoid arthritis is a systemic condition where the immune system malfunctions and attacks healthy joint tissue. To try and help alleviate the symptoms of arthritis, eat a healthy diet rich in antioxidants which can help reduce inflammation and keep your weight down (which can help avoid putting additional pressure on joints). Low-impact exercise can help to not only maintain a healthy weight, but also keeps joints flexible and strengthens the muscles that support them. Alternate between cold treatments (i.e., applying ice) to reduce joint swelling, and hot treatments (i.e., leisurely warm showers, moist heating pads) to ease stiffness in joints. Acupuncture, meditation, massage, and relaxation techniques may also help you deal with pain more easily. Don’t ignore possible signs of arthritis in your feet including hammertoes, stiffness, pain, or a callus on the inside of the big toe, swollen toes, heel pain, and shoes that suddenly become uncomfortable. If you are experiencing any of these symptoms, schedule an appointment with a podiatrist for a full examination and evaluation
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact one of our podiatrists from North Bay Ankle & Foot Center. Our doctors can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
Arthritis is a term that is commonly used to describe joint pain. The condition itself can occur to anyone of any age, race, or gender, and there are over 100 types of it. Nevertheless, arthritis is more commonly found in women compared to men, and it is also more prevalent in those who are overweight. The causes of arthritis vary depending on which type of arthritis you have. Osteoarthritis for example, is often caused by injury, while rheumatoid arthritis is caused by a misdirected immune system.
Symptoms
- Swelling
- Pain
- Stiffness
- Decreased Range of Motion
Arthritic symptoms range in severity, and they may come and go. Some symptoms stay the same for several years but could potentially get worse with time. Severe cases of arthritis can prevent its sufferers from performing daily activities and make walking difficult.
Risk Factors
- Occupation – Occupations requiring repetitive knee movements have been linked to osteoarthritis
- Obesity – Excess weight can contribute to osteoarthritis development
- Infection – Microbial agents can infect the joints and trigger arthritis
- Joint Injuries – Damage to joints may lead to osteoarthritis
- Age – Risk increases with age
- Gender –Most types are more common in women
- Genetics – Arthritis can be hereditary
If you suspect your arthritis is affecting your feet, it is crucial that you see a podiatrist immediately. Your doctor will be able to address your specific case and help you decide which treatment method is best for you.
If you have any questions, please feel free to contact our offices located in Petaluma and Sonoma, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
How to Care for Your Arthritic Foot
Arthritis is an inflammation of the joints and it can occur at any joint in the body, especially in the foot. It generally effects those who are older, however, it can occur at any age. Although there are many different forms of arthritis, there are three main types that occur in the foot. The three types are osteoarthritis, rheumatoid arthritis, and gout.
The primary cause of osteoarthritis is aging. As you age, cartilage degenerates around the joints which causes friction and pain. Obesity can cause osteoarthritis through mechanical stress. Injuries that damage joints can increase the probability as well. Finally, a family history of osteoarthritis can also increase chances of having it.
Rheumatoid arthritis occurs when the immune system attacks the joint linings and weakens them over a long time. While there is no known cause of rheumatoid arthritis, obesity and smoking can increase your chances of getting it. Women are also more likely to get it than men.
Gout is a form of arthritis that occurs when there is too much uric acid in your blood and painful crystals form in your joints. Men are more likely to have gout than women. People who are obese or drink alcohol often are also more likely to develop gout. Furthermore, having diabetes, heart disease, high blood pressure, high cholesterol, gastric bypass surgery or a family history of gout may increase your likelihood of developing the condition.
Symptoms of arthritis include pain, stiffness, swelling in the joints. These symptoms can make it harder and more painful to walk. Physical activity can increase pain and discomfort. Furthermore, joint pain can worsen throughout the day for osteoarthritis. Gout attacks generally last several days with the first few being the worst.
Diagnosis of gout includes either a joint fluid test or a blood test. X-ray imaging can detect osteoarthritis but not gout. On the other hand, there is no blood test for osteoarthritis. Rheumatoid arthritis is difficult to diagnosis. Doctors utilize family and personal medical history, a physical examination, and antibody blood tests to determine if you have rheumatoid arthritis.
Treatment varies for the different kinds of arthritis. Anti-inflammatory medication or steroids can help reduce pain from inflammation of the joints. Changing shoe types can help with some symptoms. Wider shoes can help with discomfort from gout and osteoarthritis. High heels should be avoided. Shoes with proper arch support and that take pressure off the ball of the foot can help with rheumatoid arthritis. Drinking lots of water can also help rid uric acid from the blood. Losing weight, improving your diet, and limiting alcohol and smoking can also help prevent or lessen the symptoms of arthritis.
If you are having trouble walking or pain in your feet, see a podiatrist to check if you have arthritis.
How Do Plantar Warts Form?
 Verrucae, also known as plantar warts, grow on the sole of the foot because of the human papillomavirus (HPV). This HPV virus that is usually the cause of plantar warts is contagious and thrives in warm moist environments such as swimming pools, changing room floors or community shower areas. Plantar warts will appear as a small growth with a tiny black dot in the center, and they can be painful when pinching the spot. These warts can grow up to a centimeter in diameter and may form into a cluster of multiple warts. Verrucae can be very painful, particularly when applying pressure on the foot. Patients who are struggling with a painful plantar wart should consult with a podiatrist to determine potential treatment and removal options.
Verrucae, also known as plantar warts, grow on the sole of the foot because of the human papillomavirus (HPV). This HPV virus that is usually the cause of plantar warts is contagious and thrives in warm moist environments such as swimming pools, changing room floors or community shower areas. Plantar warts will appear as a small growth with a tiny black dot in the center, and they can be painful when pinching the spot. These warts can grow up to a centimeter in diameter and may form into a cluster of multiple warts. Verrucae can be very painful, particularly when applying pressure on the foot. Patients who are struggling with a painful plantar wart should consult with a podiatrist to determine potential treatment and removal options.
Plantar warts can be very uncomfortable. If you need your feet checked, contact one of our podiatrists from North Bay Ankle & Foot Center. Our doctors will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact our offices located in Petaluma and Sonoma, CA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Warts
Plantar warts are growths that typically appear on the heels or other weight-bearing areas of the feet. These warts are caused by the human papillomavirus (HPV). The virus enters the body through breaks in the skin, such as cuts, that are on the bottom of the feet. Plantar warts are more likely to affect children and teenagers, people with weakened immune systems, people who have a history with plantar warts, and people who walk barefoot in environments exposed to a wart-causing virus.
If you suspect you have plantar warts, you may have the following symptoms: pain or tenderness while walking, a lesion that interrupts the ridges in the skin of your foot, small fleshy lesions on the bottom of the foot, or a callus where a wart has grown inward over a well-defined spot on the skin.
HPV causes plantar warts to form and is very common. There are more than 100 kinds of the virus in existence. However, only a few of them cause warts on the feet. The other types of HPV are likely to cause warts on other parts of the body.
If you have plantar warts, your podiatrist may try different treatment methods depending on your specific case. Some treatments for plantar warts are peeling medicines (salicylic acid), freezing medicines (cryotherapy), or surgical procedures. Laser treatments and vaccines are also used to treat plantar warts.
Are Foot Fractures Common?
 The foot is made up of 26 bones, so perhaps it comes as no surprise that foot fractures account for about 10% of all broken bones in the body. Foot fractures are some of the most common podiatric injuries, particularly among athletes. A broken foot bone can be especially debilitating, as the feet carry the weight of the whole body. The symptoms of a broken foot include pain, bruising, swelling, and tenderness, as well as difficulty standing or walking. The extent of your symptoms will depend on the type of fracture and its severity. A stress fracture, which is characterized by tiny cracks in the affected bone, may be less painful than a full fracture, in which a bone breaks completely. If you suspect that you may have a broken bone in your foot, please seek the care of a podiatrist.
The foot is made up of 26 bones, so perhaps it comes as no surprise that foot fractures account for about 10% of all broken bones in the body. Foot fractures are some of the most common podiatric injuries, particularly among athletes. A broken foot bone can be especially debilitating, as the feet carry the weight of the whole body. The symptoms of a broken foot include pain, bruising, swelling, and tenderness, as well as difficulty standing or walking. The extent of your symptoms will depend on the type of fracture and its severity. A stress fracture, which is characterized by tiny cracks in the affected bone, may be less painful than a full fracture, in which a bone breaks completely. If you suspect that you may have a broken bone in your foot, please seek the care of a podiatrist.
A broken foot requires immediate medical attention and treatment. If you need your feet checked, contact one of our podiatrists from North Bay Ankle & Foot Center. Our doctors can provide the care you need to keep you pain-free and on your feet.
Broken Foot Causes, Symptoms, and Treatment
A broken foot is caused by one of the bones in the foot typically breaking when bended, crushed, or stretched beyond its natural capabilities. Usually the location of the fracture indicates how the break occurred, whether it was through an object, fall, or any other type of injury.
Common Symptoms of Broken Feet:
- Bruising
- Pain
- Redness
- Swelling
- Blue in color
- Numbness
- Cold
- Misshapen
- Cuts
- Deformities
Those that suspect they have a broken foot shoot seek urgent medical attention where a medical professional could diagnose the severity.
Treatment for broken bones varies depending on the cause, severity and location. Some will require the use of splints, casts or crutches while others could even involve surgery to repair the broken bones. Personal care includes the use of ice and keeping the foot stabilized and elevated.
If you have any questions please feel free to contact our offices located in Petaluma and Sonoma, CA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Causes, Symptoms, and Treatment for a Broken Foot
One out of ten broken bones is reported to be in the feet. When an object crushes, bends, or stretches the bone beyond acceptable ranges, bones break. A break in the foot is either a fracture or a straight break.
The location of any break can tell you how the break happened. Toes, for instance, break typically as a result of something being kicked hard and with great force. Heel breaks almost always are a result of an improper landing from a tall height. Twists or sprains are the other two frequent occurrences. As with all usual breaks, they result from unexpected accident or sudden injury. As with stress fractures, breaks form as a process over time from repeated stress on already present cracks. Runners, dancers, and gymnasts are the usual athletes who receive this type of break. Stress fractures result from incredible pressure on the feet. It is no surprise these athletes bear the majority of reported fractures.
Pain, swelling, bruising, and redness are all indicative of the typical symptoms from a broken foot. Severe pain—to the point of not being able to walk—usually depends on the location of the break in the foot. Toes are on the lower scale of pain threshold, but heels are high, as are a few other particular bones. As the severity of the broken foot increases, symptoms like blueness, numbness, misshaping of the foot, cuts, or deformities will become apparent. These symptoms indicate the need to see a medical professional with access to an x-ray facility.
Prior to seeing a specialist, precautions should be taken to reduce pain and swelling. Elevate and stabilize the foot, and refrain from moving it. Immobilization of the foot is the next priority, so creating a homemade splint is acceptable. Keep in mind that while creating a splint, any increase of pain or cutting off blood circulation means that the splint should be removed immediately. Use ice to decrease swelling and relieve pain symptoms.
When dealing with a medical center, the patient should note that the treatment can vary. The treatment will depend on the severity of the fracture and the cause of the break. Crutches, splits, or casts are common treatments while surgery has been known to be used in more severe cases in order to repair the break in the bones.
Morton's Neuroma
A neuroma is a thickening of nerve tissue and can develop throughout the body. In the foot, the most common neuroma is a Morton’s neuroma; this typically forms between the third and fourth toes. The thickening of the nerve is typically caused by compression and irritation of the nerve; this thickening can in turn cause enlargement and, in some cases, nerve damage.
Neuromas can be caused by anything that causes compression or irritation of the nerve. A common cause is wearing shoes with tapered toe boxes or high heels that force the toes into the toe boxes. Physical activities that involve repeated pressure to the foot, such as running or basketball, can also create neuromas. Those with foot deformities, such as bunions, hammertoes, or flatfeet, are more likely to develop the condition.
Symptoms of Morton’s neuroma include tingling, burning, numbness, pain, and the feeling that either something is inside the ball of the foot or that something in one’s shoe or sock is bunched up. Symptoms typically begin gradually and can even go away temporarily by removing one’s shoes or massaging the foot. An increase in the intensity of symptoms correlates with the increasing growth of the neuroma.
Treatment for Morton’s neuroma can vary between patients and the severity of the condition. For mild to moderate cases, padding, icing, orthotics, activity modifications, shoe modifications, medications, and injection therapy may be suggested or prescribed. Patients who have not responded successfully to less invasive treatments may require surgery to properly treat their condition. The severity of your condition will determine the procedure performed and the length of recovery afterwards.
Why Wearing Flip-flops Regularly Can Be Bad For Your Feet
Flip-flops are easy to slip on and look great with your summer wardrobe. While they do have their place on the beach, around the pool, inside public locker rooms and showers, or outside getting the mail or letting the dog out, wearing them as regular footwear on a daily basis can ultimately be harmful to your body. Since flip-flops offer absolutely no arch support, over time you could develop pain in your arches, ankles, and knees. Flip-flops also offer scant cushioning and little support from the hard surface of the ground below which may eventually lead to heel pain and even plantar fasciitis—when the tissue connecting the bottom of your heel with your toes becomes stressed and damaged. Also, in order to keep the flip-flop on your feet, you instinctively curl your toes which changes how you walk and puts undue strain on your feet and lower back. A podiatrist can offer additional information on proper footwear and also treat any foot and ankle pain you may be experiencing.
Flip-flops are not always the best choice of footwear. If you have any concerns about your feet or ankles, contact one of our podiatrists from North Bay Ankle & Foot Center. Our doctors will assist you with all of your foot and ankle needs.
Flip-Flops and Feet
When the weather starts warming up, people enjoy wearing flip-flops. Flip-flops are comfortable, stylish, and easy to slip on and off; they're perfect for any summer beach goer. However, these shoes can cause harm to the feet.
How Can Flip-Flops Affect Me Long-Term?
- Ankle problems
- Hip problems
- Lower back problems
- Pain in the balls of the feet
- Problems with foot arches
- Changes in the way you walk
Are There Injuries Associated with Flip-Flops?
Yes. Since flip-flops are relatively weak and do not provide the same amount of support as sneakers, people who wear flip-flops regularly are more susceptible to injuries. On top of that, the open nature of the shoe makes your feet more prone to other problems, such as cuts and even infections. Common injuries and ailments include:
- Sprained ankles
- Blisters
- Infections
- Cuts and Scrapes
I like Wearing Flip-Flops. Are There Safe Alternatives?
When buying flip-flops, try to find ones that have sturdy soles and that are made of high-quality materials that will support for your feet. These flip-flops will cost more but will also last longer as a result.
If you have any questions please feel free to contact our offices located in Petaluma and Sonoma, CA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Flipping Out About Flip Flops
Although it may be tempting to wear flip-flops in warm weather, they are not the best choice of footwear for your feet. Flip-flops may be ideal for the beach, pool, spa, and shared showers, but you should avoid wearing them unless it is completely necessary.
Flip-flops only have a small strip of fabric holding your foot in place, but your toes need a better grip to keep your foot in place. The repetitive gripping can lead to an overuse of your muscles, which could result in tendinitis. This is only one of the many problems that stem from wearing flip-flops too often.
Flip flops aren’t good for extensive walking because they fail to offer arch support, heel cushioning, or shock absorption. As a result, people who wear flip flops are at a higher risk of experiencing an ankle sprain. Additionally, these shoes offer little protection for your feet, putting those who wear them at a greater risk for stubbed toes, glass cuts, and puncture wounds.
Although flip flops aren’t recommended for everyday use by anyone, it is especially important for diabetics to avoid them. A diabetic foot injury can easily become very serious, and it may even lead to amputation.
If you are experiencing pain from wearing flip-flops, you shouldn’t be hesitant to replace them with a more comfortable shoe that offers more support. If your flip-flop foot pain doesn’t go away, you should seek assistance from a podiatrist right away. It is possible that you may have a more serious foot problem such as a stress fracture or arthritis.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures are small breaks in the bone that are caused by repetitive stress. They typically occur due to overuse, forcing the bones of the foot or ankle to continually absorb the full impact of each step taken. Stress fractures can also be caused by abnormal foot structure, osteoporosis, bone deformities, or wearing improper footwear during exercise.
Stress fractures are common for individuals whose daily activities cause high levels of impact on their feet and ankles. Those who run, play tennis or basketball, or practice gymnastics tend to experience these fractures more frequently. Anyone is susceptible to this problem, though. Individuals who are normally sedentary and suddenly begin an intense, high impact workout may sustain stress fractures. This is because their muscles are not yet strong enough to handle and cushion the intensity of their activity. Osteoporosis may also cause someone to get stress fractures, because the disease weakens an afflicted person's bones and makes it easier for them to break down.
Pain from stress fractures typically occurs in the general area of the fracture. Pain can also manifest as “pinpoint pain” or pain that is felt when the site of the injury is touched, and can be accompanied by swelling. It may occur during or after activity, and it may disappear while resting and return when standing or moving. Engaging in any kind of activity, high impact or otherwise, will aggravate the pain. If the intensity of the activity increases before the stress fracture has properly healed, it can cause a full fracture.
Treatment can vary depending on the individual and the degree of injury. The primary way to treat a stress fracture is to rest the hurt foot. Some fractures will heal quickly with only a little bit of rest, while others may require a long rest period and the use of crutches, immobilization, or physical therapy. Under certain circumstances, surgery may be required to install support pins around the fracture to assist in healing.
If you are undergoing a new exercise regimen in running or some other kind of high impact activity, set incremental goals on a weekly basis so you can build up muscle strength. Make sure to wear supportive shoes to better protect you feet.
If you begin to experience any symptoms of stress fractures, you should stop exercising and rest. If the symptoms persist, consult with your podiatrist. Remembering these tips can help you prevent stress fractures to your foot and ankle, and allow you to continue living normally.